A network of tubes, called ducts, connects the liver, gallbladder, and small intestine. This network begins in the liver, where many small ducts collect bile (a fluid made by the liver to break down fats during digestion). The small ducts come together to form the right and left hepatic ducts, which lead out of the liver. The two ducts join outside the liver and develop the common hepatic duct. The cystic duct connects the gallbladder to the common hepatic duct. Bile from the liver passes through the hepatic ducts, common hepatic ducts, and into the small intestine. A small amount of bile passes through the cystic duct and is stored in the gallbladder.
When food is being digested, bile from the liver and the gallbladder is released and passes through the common bile duct and into the small intestine.
Anatomy of the intrahepatic and extrahepatic bile ducts. Intrahepatic bile ducts are a network of small tubes that carry bile inside the liver. The smallest ducts, called ductules, come together to form the right hepatic bile duct and the left hepatic bile duct, which drain bile from the liver. Bile is stored in the gallbladder and released when food is digested.
Bile duct cancer is a rare disease in which malignant (cancer) cells form in the bile ducts, so consult a bile duct cancer specialist in Houston if you experience any symptoms.
There are two types of bile duct cancer:
-
Intrahepatic bile duct cancer: This type of cancer forms in the bile ducts inside the liver. Only a small number of bile duct cancers are intrahepatic. Intrahepatic bile duct cancers are also called intrahepatic cholangiocarcinoma.
-
Extrahepatic bile duct cancer: The extrahepatic bile ducts are made up of the hilar region (at or near the fork of the left and right bile duct) and the distal region (the lower end of the bile duct). Cancer can form in either region:
The risks of bile duct cancer
Anything that increases your risk of getting a disease is called a risk factor. Having a risk factor does not mean that you will get cancer; not having risk factors does not mean you will not.
Risk factors for bile duct cancer include the following conditions:
- Primary sclerosing cholangitis (a progressive disease in which the bile ducts become blocked by inflammation and scarring).
- Chronic ulcerative colitis.
- Cysts in the bile ducts (cysts block the flow of bile and can cause swollen bile ducts, inflammation, and infection).
- Infection with a Chinese liver fluke parasite.
Signs of bile duct cancer include jaundice and pain in the abdomen
Bile Duct Cancer Specialist In Houston
These and other signs and symptoms may be caused by bile duct cancer or other conditions. Download the app Obur Health PA for services of health care in Houston and request a free consultation provided by a specialist if you have the following:
- Jaundice (yellowing of the skin or whites of the eyes). Bile duct cancer causes these ducts to narrow and block or slow the flow of bile, causing jaundice.
- Dark Tea-colored urine.
- Clay colored stool.
- Pain in the abdomen.
- Fever.
- Itchy skin.
- Nausea and vomiting.
- Weight loss for an unknown reason.
Tests that examine the bile ducts and nearby organs are used to detect (find), diagnose, and stage bile duct cancer
Staging is used to determine if cancer cells have spread within and around the bile ducts or to distant body parts.
To plan treatment, it is essential to know if the bile duct cancer can be removed by surgery.
According to the bile duct cancer specialist in Texas following tests and procedures may be used:
-
Physical exam and history: An exam of the body to check general signs of liver disease such as jaundice or skin marks resulted from itching. A history of the patient’s habits, and past illnesses and treatments will also be taken.
-
Liver function tests: A procedure in which a blood sample is checked to measure the amounts of bilirubin and alkaline phosphatase released into the blood by the liver. A higher than normal amount of these substances can be a sign of liver disease that may be caused by bile duct cancer.
-
Laboratory tests: Medical procedures that test samples of tissue, blood, urine, or other substances in the body. These tests help to diagnose disease, plan and check treatment, or monitor the disease over time.
-
Tumor markers: A sample of blood is checked to measure the amounts of certain substances made by tissues, or tumor cells in the body. These are linked to specific types of cancer when found in increased levels in the body, and are called Tumor Markers. Higher than normal levels of carcinoembryonic antigen (CEA) and CA19-9 may mean there is bile duct cancer.
-
Ultrasound exam: To detect any signs of bile duct obstruction.
-
CT scan (CAT scan): The pictures are made by a computer linked to an x-ray machine. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly.
-
MRI (magnetic resonance imaging): A procedure that uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the body. This procedure is also called nuclear magnetic resonance imaging (NMRI).
-
MRCP (magnetic resonance cholangiopancreatography): An MRI designated to visualize the Bile duct, gall bladder and the pancreatic duct only
Different procedures may be used to obtain a tissue sample and diagnose bile duct cancer
Cells and tissues are removed during a biopsy to be viewed under a microscope by a pathologist to check for signs of cancer. Different procedures may be used to obtain the sample of cells and tissue. The type of procedure used depends on whether the patient is well enough to have surgery.
Types of biopsy procedures include the following:
-
Laparoscopy: A surgical procedure to look at the organs inside the abdomen, such as the bile ducts and liver, to check for signs of cancer. Under general anesthesia, small incision (cuts) are made in the wall of the abdomen and a laparoscop (a thin, lighted tube) is inserted into one of the incisions. Other instruments may be inserted through the same or other incisions to perform procedures such as taking tissue samples to be checked for signs of cancer.
-
Percutaneous transhepatic cholangiography (PTC): A procedure used to x-ray the liver and bile ducts. Under local of general anesthetics, a thin needle is inserted through the skin below the ribs and into the liver. Dye is injected into the liver or bile ducts and an x-ray is taken. A sample of tissue is removed and checked for signs of cancer. If the bile duct is blocked, a thin, flexible tube called a stent may be left in the liver to drain bile into the small intestine or a collection bag outside the body. This procedure may be used when a patient cannot have surgery, or the bilirubin is too high prior to surgery.
-
Endoscopic retrograde cholangiopancreatography (ERCP): Again, under sedation, a procedure used to x-ray the bile ducts. An endoscope is passed through the mouth and stomach and into the small intestine. Dye is injected through the endoscope (thin, tube-like instrument with a light and a lens for viewing) into the bile ducts and an x-ray is taken. A sample of tissue is removed and checked for signs of cancer. If the bile duct is blocked, a thin tube may be inserted into the duct to unblock it and relieve the jaundice. This tube (or stent) may be left in place to keep the duct open.
-
Endoscopic ultrasound (EUS): A procedure in which an endoscope is inserted into the stomach through the mouth. An endoscope is a thin, tube-like instrument with a light and a lens for viewing. A probe at the end of the endoscope is used to bounce high-energy sound waves (ultrasound) off internal tissues or organs and make echoes. The echoes form a picture of body tissues called a sonogram. A sample of tissue is removed and checked for signs of cancer at the same time. This procedure is also called endosonography.
Certain factors affect prognosis (chance of recovery) and treatment options.
The prognosis (chance of recovery) and treatment options depend on the following:
- Whether the cancer is in the upper or lower part of the bile duct system.
- The stage of the cancer (whether it affects only the bile ducts or has spread to the liver, lymph node, or other places in the body).
- Whether the cancer has spread to nearby nerves or veins.
- Whether the cancer can be completely removed by surgery.
- Whether the patient has other conditions, such as primary sclerosing cholangitis.
- Whether the level of CA 19-9 is higher than normal.
- Whether the cancer has just been diagnosed or has recurred (come back).
The results of diagnostic and staging tests are used to find out if cancer cells have spread.
The process used to find out if cancer has spread to other parts of the body is call staging. For bile duct cancer, the information gathered from test and procedures is used to plan treatment, including whether the tumor can be removed by surgery.
There are three ways that cancer spreads in the body.
Cancer can spread through tissue, the lymphatic channels, and the blood:
- Tissue. The cancer spreads from where it began by growing into nearby areas.
- Lymph system. The cancer spreads from where it began by getting into the lymph system. The cancer travels through the lymph vessels to other parts of the body.
- Blood. The cancer spreads from where it began by getting into the blood. The cancer travels through the blood vessels to other parts of the body.
Cancer may spread from where it began to other parts of the body.
When cancer spreads to another part of the body, it is called metastasis. Cancer cells break away from where they began (the primary tumor) and travel through the lymph system or blood. The metastatic tumor is the same type of cancer as the primary tumor. For example, if bile duct cancer spreads to the liver, the cancer cells in the liver are actually bile duct cancer cells.
The following are used to plan treatment:
Resectable (localized) bile duct cancer
The cancer is localized to the area, such as the lower part of the common bile duct or perihilar area, where surgery can remove it altogether.
Unresectable, metastatic, or recurrent bile duct cancer
Unresectable cancer cannot be entirely removed by surgery. Some patients with bile duct cancer cannot have their cancer completely removed by surgery because it has spread to other organs or invaded nearby vital structures, such as the main blood vessels
Recurrent bile duct cancer has recurred (come back) after removal. Cancer may come back in the bile ducts, liver, or gallbladder. Less often, it may come back in distant parts of the body.
Bile Duct Cancer Treatment Option Overview
Three types of standard treatment are used:
Surgery
The following types of surgery are used to treat bile duct cancer:
- Removal of the bile duct: A surgical procedure to remove part of the bile duct if the tumor is small and in the bile duct only. Lymph nodes are removed and tissue from the lymph nodes is viewed under a microscope to see if there is cancer.
- Partial hepatectomy: A surgical procedure in which the part of the liver where cancer is found is removed. The part removed may be a wedge of tissue, an entire lobe, or a larger part of the liver, along with some normal tissue around it.
- Whipple procedure: A surgical procedure in which the head of the pancreas, the gallbladder, part of the stomach, part of the small intestine, and the bile duct are removed. Enough of the pancreas is left to make digestive enzymes and insulin.
After the doctor removes all cancer that can be seen during the surgery, some patients may be given chemotherapy or radiation therapy to kill any cancer cells left. Treatment given after the surgery to lower the risk that cancer will come back is called adjuvant therapy.
The following types of palliative surgery may be done to relieve symptoms caused by a blocked bile duct and improve quality of life:
-
Biliary bypass: A biliary bypass may be done if cancer blocks the bile duct and bile is building up in the gallbladder and the liver. During this operation, the surgeon will remove the gallbladder, divide the bile duct in the area before the blockage, and sew it to the small intestine to create a new pathway around the blocked area.
-
Endoscopic stent placement: If the tumor is blocking the bile duct, an Endoscopic procedure called ERCP may be done by a GI doctor to put in a stent (a thin tube) to drain bile that has built up in the area. This procedure is usually done under sedation, and you go home the same day.
-
Percutaneous transhepatic biliary drainage: A procedure used to x-ray the liver and bile ducts. A thin needle is inserted through the skin below the ribs and into the liver under local anesthetic. Dye is injected into the liver or bile ducts, and an x-ray is taken. If the bile duct is blocked, a thin, flexible tube called a stent may be left in the liver to drain bile into the small intestine or a collection bag outside the body. An interventional radiologist usually does this procedure.
Radiation therapy
Radiation therapy is a cancer treatment that uses high-energy x-rays or other types of radiation to kill cancer cells or keep them from growing.
There are two types of radiation therapy:
- External radiation therapy uses a machine outside the body to send radiation toward the cancer.
- Internal radiation therapy uses a radioactive substance sealed in needles, seeds, wires, or catheters that are placed directly into or near the cancer.
External and internal radiation therapy is used to treat bile duct cancer.
It is unknown whether external radiation therapy helps treat bile duct cancer. In unresectable, metastatic, or recurrent bile duct cancer, new ways to improve the effect of external radiation therapy on cancer cells are being studied:
-
Hyperthermia therapy: A treatment in which body tissue is exposed to high temperatures to make cancer cells more sensitive to the effects of radiation therapy and certain anticancer drugs.
-
Radiosensitizers: Drugs that make cancer cells more sensitive to radiation therapy. Combining radiation therapy with radiosensitizers may kill more cancer cells.
Chemotherapy
Chemotherapy is a cancer treatment that uses drugs to stop the growth of cancer cells, either by killing the cells or preventing them from dividing. When chemotherapy is taken by mouth or injected into a vein or muscle, the drugs enter the bloodstream and can reach cancer cells throughout the body (systemic chemotherapy).
Systemic chemotherapy treats unresectable, metastatic, or recurrent bile duct cancer. It is not yet known whether systemic chemotherapy helps treat bile duct cancer.
New types of treatment are being tested in clinical trials
Information about clinical trials is available from the
NCI website.
Liver transplant
A liver transplant removes the entire liver and replaces it with a healthy, donated liver. A liver transplant may be done in patients with peri-hilar bile duct cancer using the strict protocol. If the patient has to wait for a donated liver, another treatment is given as needed.
However, Liver transplantation is not recommended due to the high recurrence rate after the transplant.
Follow Up Tests May Be Needed
Some of the tests done to diagnose cancer or determine the stage of cancer may be repeated. Some tests will be repeated to see how well the treatment is working. Decisions about whether to continue, change or stop treatment may be based on the results of these tests.
Some tests will continue to be done from time to time after treatment ends. The results of these tests can show if your condition has changed or if cancer has recurred (come back). These tests are sometimes called follow-up tests or check-ups.
Next steps
If you need further information and obtain a second opinion please download the app "Obur Health PA" from the App Store or call
832-730-4479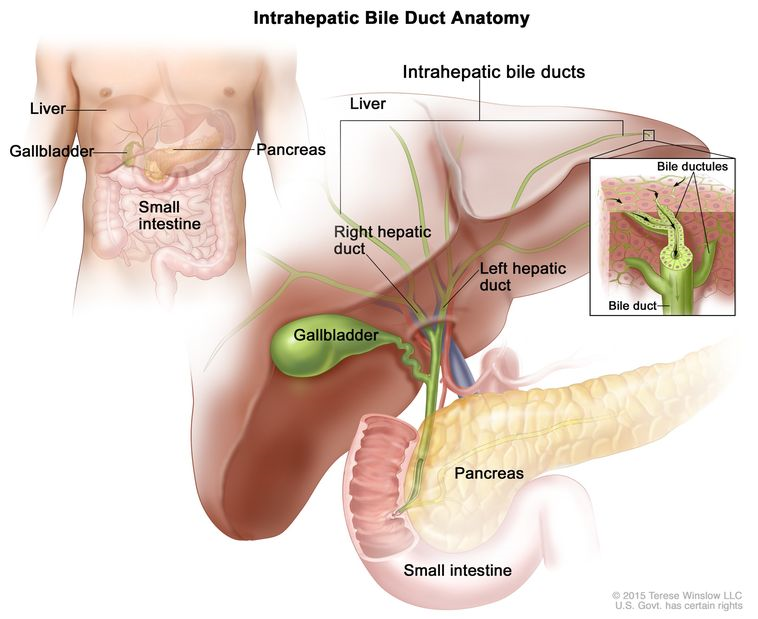
 or call 832-730-4479
or call 832-730-4479